The threat of infectious diseases looms large in Cox’s Bazar Rohingya refugee camps as well as the local communities and beyond with hardly any sign of the Myanmar nationals going back anytime soon.
Experts fear that the bordering district, where more than six lakh refugees are sheltered in overcrowded camps lacking pure water and sanitation facilities, is faced with a long-term public health challenge.
The persecuted minority group is very much vulnerable to diseases like TB, measles, AIDS, cholera and hepatitis as most of them barely got proper healthcare and vaccination back in their homeland.
The refugees here can easily mix with locals and visit marketplaces, hospitals and mosques and it is likely that the infectious diseases carried by a section of them will affect others as well.
Dodging law enforcers, Rohingyas are also going to Cox’s Bazar town, Chittagong, Chittagong Hill Tracts and other districts to join their relatives who had come to Bangladesh in previous years.
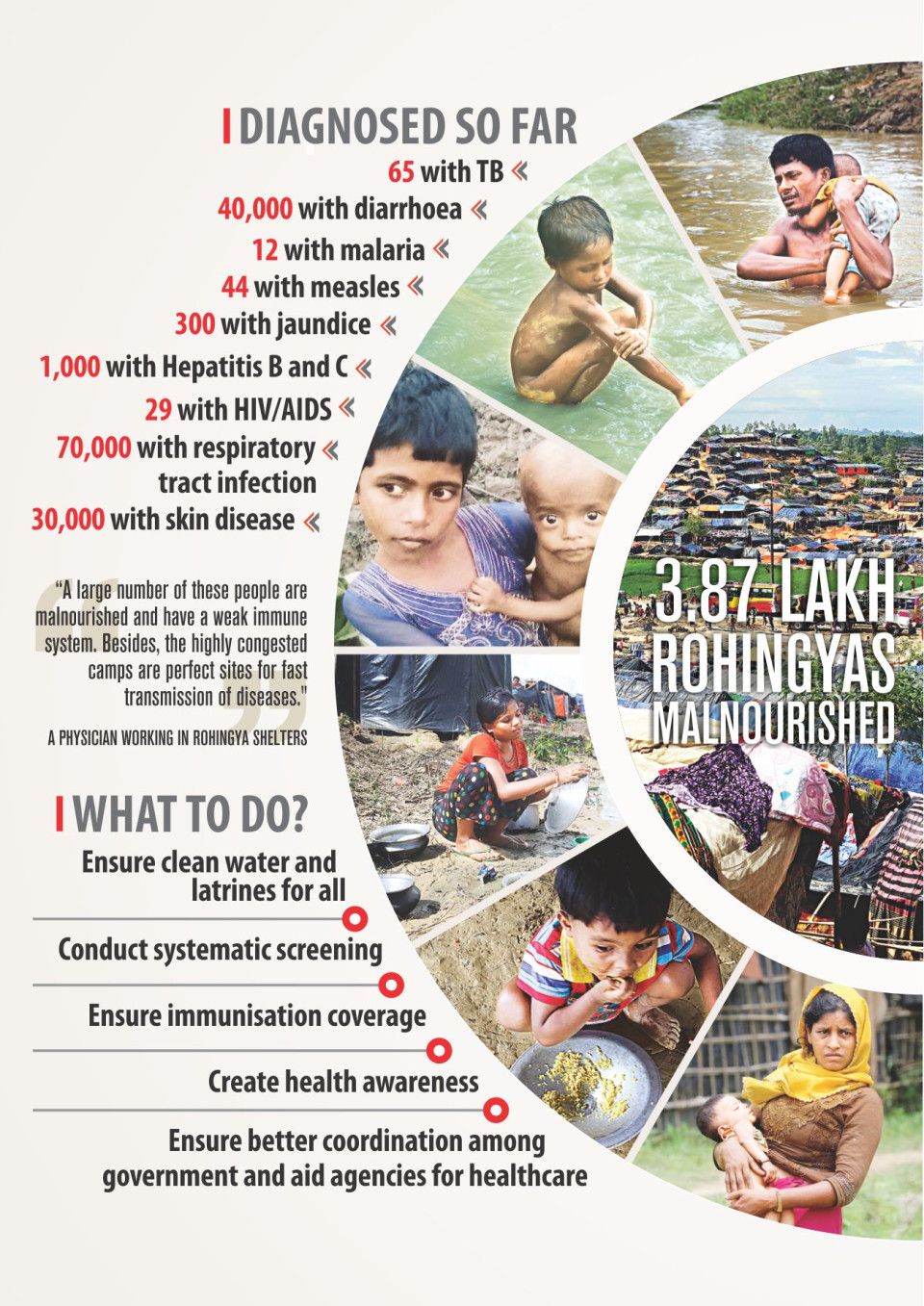
“A large number of these people are malnourished and have a weak immune system. Besides, the highly congested camps are perfect sites for fast transmission of diseases,” said physician of an international NGO working in the Rohingya shelters.
Of those who crossed over from Myanmar fleeing a brutal military crackdown in Rakhine State since August 25, about 3.87 lakh suffer from malnutrition, according to Inter Sector Coordination Group (ISCG), which coordinates the operation of different agencies in the refugee shelters.
Cox’s Bazar Civil Surgeon Dr Abdus Salam on Sunday said a total of 3.47 lakh Rohingyas so far received treatment at different health centres.
Of them, 65 were diagnosed with TB, 12 with malaria, 44 with measles, 300 with jaundice, 1,000 with Hepatitis B and C, 29 with HIV/AIDS, 70,000 with respiratory tract infection, 40,000 with diarrhoea, 30,000 with skin disease and 9,000 with injuries.
The rest got treatment for other diseases.
They were diagnosed based on suspicion and any systematic screening will surely find many more cases, he noted.
A total of 50 medical teams of the government, UN or NGOs are working in and around the camps. Patients are also seeking services from local government facilities.
“Every day, around 2,000 patients with respiratory tract infection and 1,700 with diarrhoea are thronging the healthcare centres,” Dr Mohiuddin Hussain Khan, health sector coordinator of the International Organisation for Migration (IOM), said on October 17.
IOM says only 27 percent of the sites are accessible by a vehicle of any kind, making delivery of aid and health services difficult.
Experts recommend systematic health screening, immunisation coverage, pure water and sanitation for all. There should be isolated units at health centres to prevent the spread of the diseases, they say.
THE RISK FACTORS
There are around nine lakh Rohingyas, including the new arrivals, in Ukhia, Teknaf and Ramu upazilas of Cox’s Bazar and Naikhyangchhari upazila of Bandarban.
Many fell sick, became weak or got hurt during their long walk from different parts of Rakhine. They had minimal or no food and they drank from open water sources on the way to border.
In the initial weeks of the latest influx, the refugees faced severe shortage of food, water, sanitation and medicine on this side of the border while many lived under the open sky amid heavy rains.
The government and aid agencies are still struggling to provide services in a systematic way as the new refugees remain scattered in Ukhia and other areas of the district.
Some 19,300 emergency latrines and 4,071 tube wells have been installed for them. However, 50 percent of the latrines are about to be filled up and they will be unusable very soon, says a report of ISCG led by IOM on Sunday.
Dr Azharul Islam, chief physician and head (hospitals) at ICDDR,B, said a recent field assessment found that many of the tube wells are close to latrines. “So there is a high possibility of faecal contamination of water.”
The number of latrines is also inadequate and some people still go for open defecation, Azharul Islam said, suggesting that distances should be maintained between latrines and tube wells.
He also recommended disinfecting the faecal waste, a source for diarrhoeal diseases including cholera.
Cholera can kill people very fast if untreated. In severe cases, it can lead to extreme dehydration and even death within hours.
Though no cholera patient has been yet found among the new refugees, IOM says, there are records of cholera outbreaks in Rohingya refugee camps in the past.
The good thing is, said Dr Azharul, the government with the help of World Health Organisation and other agencies have vaccinated refugees.
According to ISCG, over 7 lakh people, including Rohingyas and locals in the areas hosting refugees, were vaccinated for cholera earlier this month.
Dr Md Toufiq Rahman, an adviser of USAID-funded Challenge TB Project, said tuberculosis that remained dormant might become active now because of malnutrition of Rohingyas and their stay in cramped camps.
TB is spread from person to person through the air. When people with lung TB cough, sneeze or spit, they propel the TB germs into the air, says WHO.
Dr Toufiq added that Hepatitis B and E also pose a high risk as the viruses are spread mostly by faecally contaminated drinking water.
Another challenge is jaundice.
A physician working in the Rohingya camp said the fact that over 300 have already been diagnosed with jaundice means it is quite prevalent in the Rohingya camps.
Dr Mohiuddin Hussain Khan of IOM said there are Rohingya women who were raped in Myanmar and this heightens the possibility that there could be more HIV/AIDS patients.
He said there have not yet been any reports of “risky behaviours” of Rohingyas women or girls with local communities. What is a matter of concern is the rate of using condoms among the refugees is low.
Dr Mohiuddin suggested massive awareness campaigns and systematic service deliveries to check the disease. All those vulnerable to HIV/AIDS need to be screened and treated, he said.
Cox’s Bazar Civil Surgeon Abdus Salam added, “There is a plan for rotavirus vaccination for diarrhoea and scaled up anti-HIV/AIDS programme. We are waiting for funds.”
Physicians are also worried about measles, an airborne disease that easily spread through coughs, sneezes, saliva or nasal secretion of those infected.
The finding of 44 with measles through random screening suggests there could be many more cases among the Rohingya children, said a physician of an international NGO in Cox’s Bazar.
The authorities vaccinated some 1.35 lakh children for measles and rubella, 72,000 children for polio, and 72,000 children received Vitamin A supplementation, but many could be left out amid continuous influx and high mobility of people.
The ISCG report said finding places for setting up more health centres remains a challenge to cater to the need of unreached population in some of the large shelters in Balukhali, Unchiprang and Kutupalong.
Experts say the health risks will continue to be high until the Rohingyas are accommodated in specific areas where healthcare and other services can be provided in a systematic manner.
Graham Eastmond, shelter sector coordinator of the ISCG, said the authorities have started developing the 3,000-acre land allocated in Balukhali to bring all the Rohingya refugees under one camp.
“Accommodating so many people in one camp again is dangerous for health. If there is a disease outbreak, it will spread fast, making it difficult for the authorities to address,” he said.
Source: The Daily Star